Protecting workers from COVID-19 during the second wave.
By Professor John Cherrie, IOM
23 September 2020
The UK is entering a second wave of COVID-19 infections, and once again, the public is being asked to follow tighter restrictions. During the first wave, there was limited knowledge about how to protect workers adequately, but new guidance from the British Occupational Hygiene Society can now help guide the correct choices.
We all know that working in the NHS or in social care is a risk factor for COVID-19 infection and that these workers are more likely to die from infection than someone in the general population. Figures from the Office for National Statistics (ONS) indicate that deaths from the infection amongst social care workers are about twice the rate of those of working-age people in the general population.
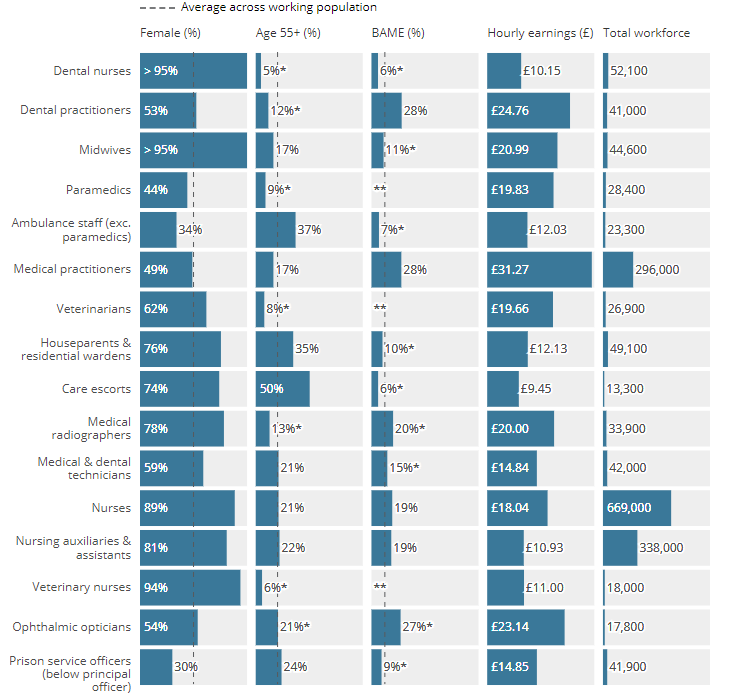
Occupations with higher exposure risks
COVID-19 also lays bare occupational inequalities, people living in socio-economically disadvantaged neighbourhoods and minority ethnic groups are disproportionately represented within lower paid ‘service’ sectors. Essentially, jobs that require a high degree of interaction with the public carry a higher disease burden.
During the first wave of the pandemic, we did a poor job of protecting workers, and we need to do things differently as we head into the winter months where typical winter flu cases increase and show signs of exacerbating the crisis.
Office for National Statistics - Characteristics of workers in highest exposure occupations:
IOM scientists help develop industry-specific guidance
If you need to find generic guidance that identifies the overall standard you need to achieve then we recommend the British Occupational Hygiene Society (BOHS) document on COVID-19: Occupation Risk Rating and Control Options According to Exposure Rank. Scientists from IOM helped develop this tool, and we are using it to advise our clients about the best strategies to minimise infection amongst their workers.
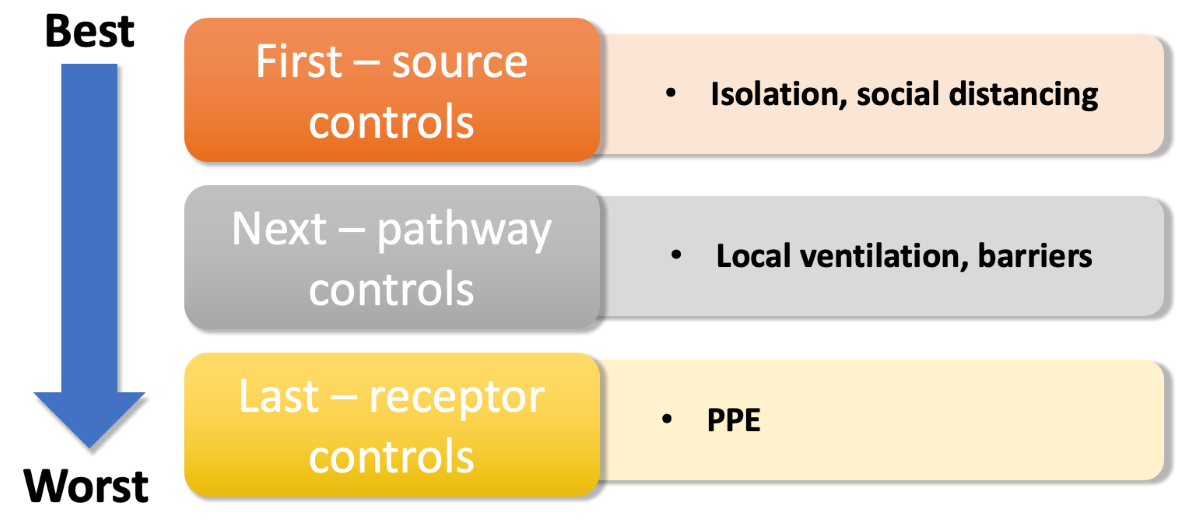
The guidance is set out in a table or matrix where the likelihood of exposure to the virus is identified and the duration of exposure categorised. This is then used to identify one of four broad strategies for controlling the virus – described as control bands in the BOHS document. The control measures are then set out in a hierarchy, with the first steps being to minimize the spread of the virus from infected people, then to reduce transmission to the worker and, finally, to think about the personal protective equipment (PPE) that should be used.
When controlling hazards PPE is considered the last line of defence, one of the big mistakes made during the first wave was to put too much reliance on PPE, which is inherently uncomfortable and often worn incorrectly. PPE is still extremely important for workplaces when all other control measures are in place. Comprehensive training and additional PPE should also be provided to ensure workers are safe under any conditions, and if any controls put in place fail.
The matrix is simple to use, and the main table contains many examples for specific groups of workers. For example, for social care workers looking after someone with COVID-19 it is recommended that:
- First: the patient is isolated, access to their room is restricted, and there is regular disinfection of surfaces near the patient,
- Next: if possible, there should be barriers or enclosure of the patient, good general ventilation in the room, regular surface disinfection away from the patient, e.g. doors or other frequent touchpoints.
- Last: as a minimum, an FFP3 respirator (the best type of disposable respirator) should be worn along with a face visor, gown, gloves and frequent hand hygiene - hand washing/sanitizing.
For a taxi driver the actions should be:
- First: require distancing and handwashing/sanitisation by the public, require customers to wear face coverings.
- Next: install a barrier between the customers and the driver, ensure regular surface disinfection of frequent touchpoints, ensure good general ventilation – open the windows, and avoid retail cash payments.
- Last: FFP2 respirators should be required for prolonged contact with customers - otherwise fluid resistant surgical masks, visor, gloves and/or hand hygiene – hand washing/sanitizing.
Workplace protection during the COVID-19 outbreak
The Workplace Protection team at IOM can work with duty holders to identify ways to minimise transmission in work and public spaces using the BOHS risk matrix tool and an IOM COVID-19 Workplace Risk Assessment.
Current emerging evidence is suggesting 4 out of 5 transmissions appear to be by aerosol transmission in indoor often poorly ventilated spaces, with the other 1 in 5 likely to be via fomite transmission (also generally indoors).
Following the UK governments central message of hands, face and space are a good starting point and duty holders should consider a series of control measures such as the use of barriers, local ventilation and wearing face masks; respirators where they are really needed and surgical type masks in all other work situations. With this type of approach, we can reduce the unacceptable infection risks for our vulnerable workers.